RELATED CHAPTERS
Escalation and Challenge Protocol
Adult Safeguarding Risk Threshold Tool
RELEVANT INFORMATION
Self-Neglect at a Glance (SCIE)
7 Minute Briefings (Adults AP, AS and AT)
What to do about self neglect – Animation (North East ADASS)
Self Neglect – Don’t walk away, walk alongside (South Tyneside leaflet)
Tissue Viability Service: Referral Criteria and Referral Form (for people of all ages with a wide variety of complex wounds, including pressure ulcers, leg ulcers and surgical wounds).
This section of the APPP contains the accessible formatted version of the Self-Neglect Guidance. You can also view a PDF version: Self Neglect Guidance for Multi Agency Partners
November 2023: This multi agency guidance for staff is new. It explains how to support someone who is self-neglecting or hoarding.
CONTENTS
1. Introduction
The purpose of this toolkit is to develop practice guidance for a range of multi-agency professionals to use, when supporting someone who is self-neglecting or hoarding. Through a review of the current self-neglect process, there has been some identified learning that can be applied in the development of this toolkit. This Toolkit can be used by any multi-agency partner.
The Care and Support Statutory Guidance clarified the relationship between self-neglect and safeguarding and has now made self-neglect a category of harm, about which the Local Authority has a duty to make enquiries and to assess need with the promotion of well-being at the heart.
Further clarification received from the Department of Health and Social Care states that self-neglect is the responsibility of safeguarding boards in terms of ensuring that policies and procedures underpin work around people who self-neglect, balancing, self-determination, robust mental capacity assessment, consent and protection. It does not mean that each case of self-neglect must progress to a Section 42 enquiry, but that each case must receive an appropriate response.
Engaging with, assessing and providing support to such people can be complex and frustrating and often requires a clear understanding of the law, to ensure actions taken are defensible. Many dedicated, compassionate practitioners are left struggling with cases, feeling alone and isolated.
In 2011, the Law Commission undertook a series of scoping studies in adult social care. This identified a historic lack of understanding of self-neglect, resulting in inconsistent approaches to support and care. In an effort to address this, the Care and Support Statutory Guidance formally recognises self-neglect as a category of abuse and neglect – and within that category identifies hoarding.
This means that the need locally for a consistent approach is key in ensuring that multi-agency professionals work together, to ensure that people who self-neglect have the right support, which is timely and in a proportionate and preventative way.
2. The Local Picture
| Year | Number of Safeguarding Concerns Raised | Number of Section 42 Enquiries | Number Relating to Self-Neglect | No/Outcome of Cases Submitted for SAR |
| 2019/20 | 952 | 787 | 32 | 3 |
| 2020/21 | 1072 | 478 | 26 | 13 |
| 2021/22 | 1084 | 361 | 32 | 13 |
| 2022/23 | 1312 | 346 | 69 | 6 |
Self-neglect became a domain of abuse within the Care Act 2014. However, how self-neglect differs from other domains of abuse, is that there is no other person inflicting self-neglect on the individual in an abusive way – therefore there is no alleged perpetrator only the individual themselves.
For social workers, this provides a significant challenge in developing relationships that empower the individual, or safety plans based upon what makes a person feel safe and well cared for, yet respect autonomous decision making, whilst juggling other duties and responsibilities.
It is important to explore the person’s history; listen to the way they talk about their life, difficulties and strategies they have developed for self-protection. By doing this, social workers and health professionals can begin assessing why the person self-neglects and begin to offer support in replacing attachment objects, with interaction and relationships with people and the community. Distress may have led people to seek comfort in having possession; when faced with isolation they may seek proximity to things they’re attached to and when faced with chaos may seek to preserve predictability.
Early relationships can have quite an effect on how a person perceives the world and may not recognise their self-neglect – and may even find comfort in their situation. Deep-seated emotional issues, which have evolved as coping strategies cannot be undone in an instant.
3. What is Self Neglect?
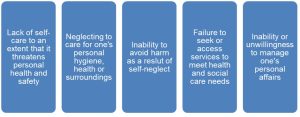
(Click on the image to enlarge it)
Self-neglect manifests itself in different ways. It might be that a person is physically or mentally unwell or has a disorder and cannot meet their own care needs as a result. They may have suffered trauma or loss or be receiving inappropriate support from a carer. The person may not recognise the level of self-neglect. The foundations of self-neglect can begin with trauma and loss, parental attachment and control issues and information processing deficits.
Self-neglect can also occur as a result of cognitive impairment, dementia, brain damage, depression or psychotic disorders. It may be down to substance use, including misuse of prescribed medications.
3.1 Types of Self-Neglect
- Lack of self-care to an extent that it threatens personal health and safety;
- Neglecting to care for one’s personal hygiene, health or surroundings;
- Inability to avoid self-harm;
- Failure to seek help or access services to meet health and social needs;
- Inability or unwillingness to manage one’s personal affairs.
3.2 Indicators of self-neglect
(Click on the image to enlarge)
3.3 Children and the links to self-neglect
The impact of self-neglect in adults can impact upon children, and present as a form of child abuse that occurs when a child’s basic needs are not met by their caregivers. This can include lack of food, clothing, hygiene, medical care, education, or supervision for children and result in parent(s) being unable to their child’s emotional needs. This can be because of mental health issues, substance or alcohol misuse, self-harm, loss and grief or any form of past and current trauma.
Practitioners should always be aware of the impact of adult self- neglect on any children living within the family home and if they are worried about a child, submit the relevant safeguarding children concerns as per guidance provided in the Safeguarding Children Partnership, Referral Guidance.
Further information can also be found at: Working Together to Safeguarding Children
3.4 Obesity / malnourishment and the links to self-neglect
There is an interface between obesity or malnourishment and self-neglect, which identifies some key issues for practitioners:
| In cases of self-neglect where the person is plus size or malnourished, staff should consider any possible underlying causes, or disabilities which may be interfering with the person’s ability and/or choice to engage with care and support. |
| Cooperation, collaboration and communication between professionals specialised in working with disability and those working in obesity/malnourishment services which can help lead to improved prevention, early detection and treatment for people. |
| Health and Social Care providers need to identify and understand the barriers that people with disabilities and obesity/malnourishment may face in access to health and preventative services and make efforts to address them before assuming that the person is ‘refusing’. |
| Health and social care providers need to adjust policies, procedures, staff training and service delivery to ensure that services are easily and effectively accessed by people with disabilities and obesity/malnourishment. This needs to include addressing problems in understanding and communicating health needs, access to transport and buildings, and tackling discriminatory attitudes among health care staff and others, to ensure that people are offered the best possible opportunity of engaging with services. |
| It may be that the person is able to engage in a conversation about a mental health or physical health problem when they do not feel able to talk about their obesity/ malnourishment. This may be due to concerns about stigma, embarrassment or worries that professionals may seek interventions that they are not ready to access. Engaging the person to work on the issues they see as important is essential to developing a longer-term relationship. |
| There should be active support for obese/malnourished individuals to live independent and healthy lives. It is important that health promotion initiatives recognise the limits of information giving and the need for whole communities to be included in tackling discrimination, to allow people to have the confidence to accept support and join in with community activities. |
4. Roles and Responsibilities
| Service | Examples of how agencies can support someone who is self-neglecting |
| Clinical Psychology | can support people who self-neglect by developing psychological understanding of their situation and helping them find strategies to help manage their situation, including psychological therapy. |
| Community nurses | provide healthcare to people in their own homes. They will refer to other services, such as the continence or respiratory service, or for specialist equipment such as profiling beds. |
| Environmental health | …aims to reduce the risk to the self-neglecting person themselves, but also the wider community through practical direct work with the person, invoking any relevant legislation where necessary. |
| Fire and Rescue Services | can provide fire safety advice, including hoarding, and put practical measures in place to reduce the risk of a fire. They may refer on to other agencies for more support. |
| General Practitioners (GPs) | can identify people who seem to be self-neglecting, provide support and advice and refer to other agencies such as mental health, to enable people to get support and assistance if required. |
| Hospital nurses | …will identify patients who seem to be self-neglecting, support the patient and refer to other agencies to enable potential to gain help and support required, within and following their stay in hospital |
| Housing | can help people practically to support their tenancies to avoid the risk of being evicted, due to problems with self-neglect. Housing will refer to other agencies if required, for example the Fire Service, Assistive Technology etc. |
| Advocacy | support the person to make their own decisions, ensure their views, wishes, feelings, beliefs and values are listened to, and may challenge decisions that they feel are not in the person’s best interests. |
| Occupational therapists | work with individuals to identify any difficulties they experience in day to day living activities, finding ways to help individuals resolve them. They support independence where possible and safety within the community, to help build confidence and motivation. |
| Paramedics | are called by the person or a third party caller due to medical concerns or health deterioration. They will deliver appropriate emergency treatment, assess mental capacity in relation to the health issues presented (particular around refusal to go to hospital) and refer on to other agencies with concerns. |
| Physiotherapists | can help with treatment of injury, disease or disorders through physical methods and interventions. A Physio helps and guides patients, prescribes treatment and orders equipment. They can refer to other services if required. |
| Police | can investigate and prosecute if there is a risk of wilful neglect, they can provide safeguarding to families and communities by sharing information, refer to specialist partner agencies and use force to gain entry/access of there are legal grounds to do so. |
| Probation | will identify problems via home visits and provide regular monitoring. They may refer to social services, mental health, housing and health. They will complete risk assessments and risk management plans, making links to the risk of serious harm. |
| RSPCA/LA/Animal Welfare Services | investigate complaints of cruelty to and neglect to animals and offer support and advice. |
| Social workers | …will complete assessments by talking to and getting to know the person. They may establish their mental capacity to make a particular decision about their lives and consider all options available. They may put in support or care or refer to other agencies. They may arrange multi-agency meetings and will rely on sign up from partner agencies regarding this. They can help with relationship building, communication skills and try to develop social networks for the person who is self-neglecting. |
| Voluntary, Community and Faith Sector organisations | staff and volunteers can provide a whole range of social opportunities and support, to support people to connect with their peers and communities. This includes clubs, support groups, foodbanks and faith led support services. Staff and volunteers from this sector are a vital part of the formal and informal planned care and support for people who self-neglect. |
| Mental health outreach team | can provide specialist mental health related to support to people who self-neglect in their own homes. This includes practical support, active support and will aim to promote independence and choice, linking in with other services and sharing information. |
| Red Cross | …can provide short term support in the home for people after a hospital admittance following an accident, illness or during a personal crisis. |
| Hospital Discharge Social Care | can assess and plan care and support for people who are admitted to hospital, so that when the person is discharged, this is as safe a journey as possible for the person who is self-neglecting. This includes completing capacity and risk assessments, as well as information sharing with the wider MDT. |
| Welfare rights | …can support the person who is self-neglecting to maximise their income, which may have a positive impact on their ability to self-care and emotional wellbeing. |
| Drug and alcohol services | can provide support, advice, counselling and ensuring the person who is self-neglect access the appropriate level of health and social care support. This in addition to supporting the person if they have a drug or alcohol problem which may impact on their ability to self care. |
| Reablement / intermediate care | can support if someone is self-neglecting due to an acute problem, by providing short term support to re-enable and promote independence. |
REMEMBER
Safeguarding is Everyone’s Responsibility and all professionals can undertake assessments, informed by multi-agency meetings where appropriate.
See also Local Contacts for information on how to contact safeguarding partners.
5. The Legal Perspective
5.1 Legal options in relation to self-neglect
There are many legislative responsibilities placed on agencies to intervene in or be involved in some way with the care and welfare of adults who are believed to be vulnerable.
It is important that everyone involved thinks proactively and explores all potential options and wherever possible, the least restrictive option e.g. a move of the person permanently to smaller accommodation where they can cope better and retain their independence.
The following outlines a summary of the powers and duties that may be relevant and applicable steps that can be taken in cases of dealing with persons who are self-neglecting and/or living in dirty and unpleasant conditions. The following is not necessarily an exhaustive list of all legislative powers that may be relevant in any particular case. Cases may involve user of a combination of the following exercise of legislative powers.
The tenant is responsible for the behaviour of everyone who is authorised to enter the property.
There may also be circumstances in which a person’s actions amount to anti-social behaviour under the Anti-Social Behaviour, Crime and Policing Act 2014. Section 2(1)(c) of the Act introduced the concept of “housing related nuisance”, so that a direct or indirect interference with housing management functions of a provider or local authority, such as preventing gas inspections, will be considered as anti-social behaviour. Injunctions which compel someone to do or not do specific activities, may be obtained under Section 1 of the Act. They can be used to get the tenant to clear the property or provide access for contractors. To gain an injunction, the landlord must show that, on the balance of probabilities, the person is engaged or threatens to engage in antisocial behaviour, and that it is just and convenient to grant the injunction for the purpose of preventing an engagement in such behaviour. There are also powers which can be used to require a tenant to cooperate with a support service to address the underlying issues related to their behaviour.
Environmental Health
Environmental Health Officers in the Local Authority have wide powers/duties to deal with waste and hazards. They will be key contributors to cross departmental meetings and planning and in some cases, e.g. where there are no mental health issues, no issues regarding the mental capacity of the person concerned, and no other social care needs, then they may be the lead agency and act to address the physical environment.
Remedies available under the Environmental Protection Act 1990 include:
- Litter clearing notice where land open to air is defaced by refuse (section 92a);
- Abatement notice where any premise is in such a state as to be prejudicial to health or a nuisance (sections 79/80)
Other duties and powers exist as follows:
- Town and Country Planning Act 1990 provides the power to seek orders for repairs to privately owned dwellings and where necessary compulsory purchase orders. The Housing Act 2004 allows enforcement actions where either a category 1 or category 2 hazard exists in any building or land posing a risk of harm to the health or safety of any actual or potential occupier or any dwelling or house in multiple occupation (HMO). Those powers range from serving an improvement notice, taking emergency remedial action, to the making of a demolition order. Local Authorities have a duty to take action against occupiers of premises where there is evidence of rats or mice, under the Prevention of Damage by Pests Act 1949;
- The Public Health (Control of Disease) Act 1984 Section 46, sets out restrictions in order to control the spread of disease, including use of infected premises, articles and actions that can be taken regarding infectious persons.
Landlords
These powers could apply in Extra Care Sheltered Schemes, Independent Supported Living, private-rented or supported housing tenancies. It is likely that the housing provider will need to prove the tenant has mental capacity, in relation to understanding their actions before legal action will be possible. If the tenant lacks capacity, the Mental Capacity Act 2005 should be used.
In extreme cases, a landlord can take action for possession of the property for breach of a person’s tenancy agreement, where a tenant fails to comply with the obligation to maintain the property and its environment to a reasonable standard. This would be under either Ground 1, Schedule 2 of the Housing Act 1985 (secure tenancies) or Ground 12, Schedule 2 of the Housing Act 1988 (assured tenancies).
The tenant is responsible for the behaviour of everyone who is authorised to enter the property.
Mental Health Act 1983
Sections 2 and 3 Mental Health Act 1983: Where a person is suffering from a mental disorder (as defined under the Act) of such a degree, and it is considered necessary for the patient’s health and safety or for the protection of others, they may be compulsorily admitted to hospital and detained there under Section 2 for assessment for 28 days. Section 3 enables such a patient to be compulsorily admitted for treatment.
Section 7 Mental Health Act 1983: A Guardianship Order may be applied for where a person suffers from a mental disorder, the nature or degree of which warrants their reception into Guardianship (and it is necessary in the interests of the welfare of the patient or for the protection of other persons). The person named as the Guardian may be either a local social services authority or any applicant.
A Guardianship Order confers upon the named Guardian the power to require the patient to reside at a place specified by them; the power to require the patient to attend at places and times so specified for the purpose of medical treatment, occupation, education or training; and the power to require access to the patient to be given, at any place where the patient is residing, to any registered medical practitioner, approved mental health professional or other person so specified.
In all three cases outlined above (i.e. Schedule 2, 3 and 7), there is a requirement that any application is made upon the recommendations of two registered medical practitioners.
Section 135 Mental Health Act 1983: Under Section 135, a Magistrate may issue a warrant where there may be reasonable cause to suspect that a person believed to be suffering from mental disorder, has or is being ill-treated, neglected or kept otherwise than under proper control; or is living alone unable to care for themselves. The warrant, if made, authorises any constable to enter, if need be by force, any premises specified in the warrant in which that person is believed to be, and, if thought fit, to remove them to a place of safety.
Section 135 lasts up to 36 hours (it’s usually 24 hours and in certain circumstances a Doctor can extend by 12 hours) and is for the purpose of removing a person to a place of safety with a view to the making of an assessment regarding whether or not Section 2, 3 or 7 of the Mental Health Act should be applied.
Section 136 Mental Health Act 1983 allows Police Officers to remove adults who are believed to be “suffering from mental disorder and in immediate need of care and control” from a public place of safety for up to 24 hours for the specified purposes, with the option to extend for 12 hours. The place of safety could be a police station or hospital.
Mental Capacity Act 2005
The powers to provide care to those who lack capacity are contained in the Mental Capacity Act 2005. Professionals must act in accordance with guidance given under the Mental Capacity Act Code of Practice when dealing with those who lack capacity and the overriding principle is that every action must be carried out in the best interests of the person concerned.
Where a person who is self-neglecting and/or living in squalor and does not have the capacity to understand the likely consequences of refusing to cooperate with others and allow care to be given to them and/or clearing and cleaning of their property, a best interest decision can be made to put in place arrangements for such matters to be addressed. A best interest decision should be taken formally with professionals involved and anyone with an interest in the person’s welfare, such as members of the family.
The Mental Capacity Act 2005 provides that the taking of those steps needed to remove the risks and provide care will not be unlawful, provided that the taking of them does not involve using any methods of restriction that would deprive that person of their liberty. However, where the action requires the removal of the person from their home, then care needs to be taken to ensure that all steps taken are compliant with the requirements of the Mental Capacity Act. Consideration needs to be given to whether or not any steps to be taken require a Deprivation of Liberty Safeguards application (see Deprivation of Liberty Safeguards chapter). In addition consideration needs to be given to S47 of the Care Act whereby the Local Authority needs to have taken reasonable steps to mitigate/prevent the loss or damage of a person’s property and/or belongings.
Where an individual resolutely refuses to any intervention, will not accept any amount of persuasion, and the use of restrictive methods not permitted under the Act are anticipated, it will be necessary to apply to the Court of Protection for an order authorising such protective measures. Any such applications would be made by the person’s care manager who would need to seek legal advice and representation to make the application.
Section 44 Mental Capacity Act 2005 created an offence of ill-treating or wilfully neglecting a person who lacks capacity, or whom the offender reasonably believes to lack capacity. The offence may only be committed by certain persons who have a caring or other specified responsibility for the person who lacks capacity. The penalties are, on summary, conviction up to 12 months imprisonment, a fine not exceeding the statutory maximum, or both, or on conviction on indictment of up to 5 years imprisonment or a fine or both.
Article 8 of the Human Rights Act 1998 states that the right to private life protects people’s well-being and autonomy, including: people living free from abuse or neglect (including self-neglect).
Court of Protection
You can apply to the Court of Protection to get an urgent or emergency court order in certain circumstances, e.g. a very serious situation when someone’s life or welfare is at risk and a decision has to be made without delay. You won’t get a court order unless the court decides it’s a serious matter with an unavoidable time limit. Where an emergency application is considered to be required, relevant legal advice must be sought.
Power of Entry
The Police can gain entry to a property if they have information that a person inside the property was ill or injured with the purpose of saving life and limb. This is a power under Section 17 of the Police and Criminal Evidence Act 1984.
Inherent Jurisdiction
There have been cases where the Courts have exercised what is called the ‘inherent jurisdiction’ to provide a remedy where it has been persuaded that is necessary, just and proportionate to do so, even though the person concerned has mental capacity. See also Mental Capacity chapter
In some cases of self-neglect, there may be evidence of some undue influence from others who are preventing public authorities and agencies from engaging with the person concerned and thus preventing the person from addressing issues around self-neglect and their environment in a positive way.
Where there is evidence that someone who has capacity is not necessarily in a position to exercise their free will due to undue influence, then it may be possible to obtain orders by way of injunctive relief that can remove those barriers to effective working. Where the person concerned has permitted another reside with them and that person is causing or contributing to the failure of the person to care for themselves or their environment, it may be possible to obtain an Order for their removal or restriction of their behaviours towards the person concerned.
In all such cases legal advice should be sought.
Animal welfare
The Animal Welfare Act 2006 can be used in cases of animal mistreatment or neglect. The Act makes it against the law to be cruel to an animal and the owner must ensure the welfare needs of the animal are met. Powers range from providing education to the owner, improvement notices, and fines through to imprisonment. The powers are usually enforced by the RSPA, Environmental Health or DEFRA.
Fire
The Fire and Rescue Service pathway states that if 3 or more of these factors are present a request / referral for a safe and well check should be made.
| Age | Behaviours | Vulnerabilities |
| Occupiers over 65 | · Smoking
· Smokes where sleeps · Clutter/Hoarding level 4 and over · Previous fires/burn marks · Alcohol and Substance Misuse · Emollients and paraffin based creams |
· Lives Alone
· Restricted Mobility · Immobile · Sensory Impairments |
6. Mental Capacity and Self Neglect
The Mental Capacity Act 2005 provides a statutory framework for people who lack capacity to make decisions for themselves. The Act has 5 statutory principles and these are the values which underpin the legal requirements of the act. They are:
- A person must be assumed to have capacity unless it is established that they lack capacity;
- A person is not to be treated as unable to decide unless all practical steps have been taken without success;
- A person is not to be treated as unable to decide merely because they make an unwise decision;
- An act done or decision made, under the Act on behalf of a person who lacks capacity must be done, or made, in their best interests;
- Before the act is done or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person’s rights and freedom of action.
Where a person’s self-neglecting behaviour poses a serious risk to their health and safety, intervention will be required. With the exception of statutory requirements, any intervention or action proposed must be with the person’s consent. In extreme cases of self-neglecting behaviour the very nature of the environment should lead professionals to question with the person has capacity to consent to the proposed action or intervention and trigger a capacity assessment.
This is confirmed by the Mental Capacity Act Code of Practice, which states that one of the reasons why people may question a person’s capacity to make a specific decision is “the person’s behaviour or circumstances cause doubt as to whether they have capacity to make a decision” (4.35 MCA Code of Practice). Consideration must be given where there is dialogue or situations that suggest a person’s capacity to make decision with regard to their place of residence or care provision may be in doubt.
Any capacity assessment carried out in relation to self-neglecting behaviour must be time specific and relate to a specific intervention or action. The professional responsible for undertaking the capacity assessment will be the person who is proposing the specific intervention or action and is referred to as the ‘decision-maker’. Although the decision maker may need to seek support from other professionals in the multi-disciplinary team, they are responsible for making the final decision about a person’s capacity.
If the person lacks capacity to consent to the specific action or intervention, then the decision maker must demonstrate that they have met the requirements of the best-interests “checklist”. Due to the complexity of such cases, multi-agency meetings to coordinate assessments may be required. Where the person denies access to professionals the person who has developed a rapport with the person self-neglecting will need to be supported by the relevant agencies to conduct capacity assessments.
In particularly challenging and complex cases, it may be necessary for the local authority to refer to the Court of Protection to make the best interests decision. Any referral to the Court of Protection should be discussed with legal services and the relevant service manager.
6.1 What is the difference between competency and capacity and why is this important when working with people who self-neglect?
Competency: To be competent means that the overall function of the brain is working effectively to enable a person to make choices, decisions and carry out functions. Often the mini mental state test is used to assess competency. In many people who have, for example, Dementia, Parkinson’s Disease or Huntington’s Disease, the first aspect of brain function affected is the executive function and unfortunately this is not tested very effectively using the mini mental state test.
Effective Function: The executive function of the brain is a set of cognitive or understanding/processing skills that are needed to plan, order, construct and monitor information to set goals or tasks. Executive function deficits can lead to problems in safety, routine behaviours. The executive functions are in the first to be affected when someone has, for example, dementia. See also Executive Functioning Grab Sheet.
Capacity: Capacity is decision making ability and a person may have quite a lack of competency but be able to make a specific decision. The decision making ability means that a person must be able to link the functional demands, the ability to undertake tasks, the ability to weigh up the risks and the ability to process the information and maintain the information to make the decision. In some way, shape or form, the person has to be able to let the person assessing them know that they are doing this. Many competent people make what others would consider to be bad decisions but are not prevented from taking risks and making bad decisions. This is not a sign that a person lacks capacity to make the decision, just that they have weighed everything up, considered the factors and determined that for them this would be what they wanted. The main issue in the evaluation of decision-making capacity is the process of making the decision, and not the decision itself.
This is important because the mental capacity assessment uses two tests. The first is called the functional test and this involves looking at whether the adult can make the decision in question. Adults should be provided with practical support to help them make decisions. If you are concerned about an adults’ ability to make decisions because either they cannot:
- understand information about the decision to be made; or
- retain that information in their mind;
- or weigh up that information as part of the decision making process:
- or communicate their decision by talking, using sign language or any other means)
Then they will be considered not able to make a decision. There only needs to be evidence in one of these areas, not all of them. If the assessment finds that the adult cannot make the decision in question, even with support, then Stage 2 should be considered.
The second part of a mental capacity assessment requires evidence to show that the person’s inability to make a decision is because of an impairment of their mind or brain. Examples include, conditions associated with some types of mental illness, dementia, significant learning difficulties, long term brain damage and the effects of drugs and alcohol. If the adult does not have such an impairment or disturbance of the mind or brain, they will not lack capacity under the Mental Capacity Act.
Decisions should not be broad decisions about care, services or treatment, they should be specific to a course of action. If a practitioner requires the consent, agreement, signature or understanding of the individual, then they should determine the capacity of the person to consent to that action using the assessment process defined in the Mental Capacity Act 2005. This may be for tenancy, individual treatment options, aspects of care offered, equipment required, access to services, information sharing or any intervention. If you understand the course of action being proposed and offered to the person, then you will be the person required to assess the individual’s the person, all agencies are responsible for developing questions for that agency to ask to determine their capacity as well as is practicably possible.
For more information, and a mental capacity assessment template, see Mental Capacity.
6.2 Practice examples
Housing: The Housing Officer will need to conduct and record a capacity assessment, where there is doubt about the person’s ability to provide consent. If the person is deemed to lack capacity to make that decision a ‘Best Interest’ decision must be made. A third party cannot sign a tenancy agreement on behalf of another person unless they have a Court Appointed Deputyship or a Lasting Power of Attorney that specified such actions under ‘finance’.
Health: If a health professional is proposing a course of treatment, medication or intervention, they understand the intervention proposed, therefore, they are the person to determine whether the person self-neglecting understands the intervention. If the health professional doubts the person’s ability to understand they must conduct (and record) a capacity assessment. If the person is deemed to lack capacity to make that decision a ‘Best Interest’ decision must be made. A third party cannot give consent on behalf of another person unless they have Court Appointed Deputyship or a Lasting Power of Attorney that specifies such actions under ‘welfare’.
Occupational Therapy: The Occupational Therapist (OT) understands the rehabilitative process/equipment required by the person to meet their needs. If the person does not appear to understand then the OT must assess the person’s capacity to decide about the proposed equipment.
6.4 Examples of what to ask when assessing capacity
6.4.1 The legal test
Section 2(1) Mental Capacity Act 2005 “A person lacks capacity in relation to a matter if, at the material time, he is unable to make a decision for himself in relation to that matter because of an impairment of, or disturbance in the functioning of, the mind or brain”.
6.4.2 Applying the test
To apply the test if can be broken down into 3 questions:
- Is the person able to decide about where to live?
- Is there an impairment or disturbance in the functioning of the person’s mind or brain? If so,
- Is the person’s inability to make the decision because of the identified impairment or disturbance?
Think about:
- What areas does the person need support with?
- What sort of support do they need?
- Who will be providing the support?
- What would happen if they did not have any support or refused it?
- That carers might not treat them properly and that they can complain if they are not happy about their care.
A person is unable to decide on residence if they are unable to:
- Understand the information relevant to the decision; or
- Retain that information; or
- Use or weight that information as part of the process of making the decision; or
- Communicate their decision (by any means).
See also Mental Capacity chapter.
If you require further information on the Mental Capacity Act please book on the multi-agency training course: Safeguarding training – South Tyneside Council.
7. Pathway for Self Neglect
View the Pathway for Self Neglect
8. When does a Section 42 (Safeguarding) Enquiry Occur?
In most safeguarding issues, the Care Act 2014 (Section 42) requires that each local authority must make enquiries, or cause others to do so, if it believes an adult is experiencing, or is at risk of, abuse or neglect. This enquiry should establish whether any action needs to be taken to prevent or stop abuse or neglect, and if so, by whom.
Cases of self-neglect may not prompt a Section 42 enquiry. We invariably judge these on a case by case basis. Whether or not a response is required will depend on the adult’s ability to protect themselves by controlling their own behaviour. There may come a point when they are no longer able to do this, without external support.
It is key to establish a trusting relationship with a person who is engaging in self-neglect because restricting their autonomy can be harmful.
What professionals think an adult who self-neglects might hope and fear when they arrive in their lives:
| I Hope that… | |||||||
| “They will listen to me” | “They will provide support” | “They will be respectful” | “They will leave me alone” | “They will help me” | |||
| “They will sort my problems out” | “They will be sensitive and understanding” | “They will see me as a person” | |||||
| “They won’t disappear or change too frequently if I’ve got to know them” | “They will manage my health and care needs” | ||||||
| I Fear That … | ||||
| “I will lose my independence” | “They will make me do things” | “They will take my things away” | “They will put me in a home” | “There will be repercussions which I will not like” |
| “I will lose control of my life” | “I will lose my identity” | “I will be arrested or prosecuted” | “I will lose my home” | “They will judge me” |
| “They will make me feel distressed, upset and anxious” | “They will evict me and I will be homeless” | |||
Safeguarding duties apply to:
- Any adult who has care and support needs (whether or not the local authority is meeting any of those needs); and
- Is experiencing, or at risk of abuse and neglect (including self-neglect); and
- As a result of those care and support needs is unable to protect themselves from either the risk or, or the experience of, abuse and neglect
The duties apply equally whether a person lacks mental capacity or not. So, while an individual’s wishes and feelings are central to their care and support, agencies must share information with the local authority for initial enquiries to take place.
Enquiries may take place even when the person has mental capacity and does not wish information to be shared, to ensure abuse and neglect is not affecting others, that a crime has not been committed, or that the person is making an autonomous decision and is not being coerced or harassed into that decision. Safeguarding duties have a legal effect in relation to many organisations and the local authority may request organisations to make further enquiries on their behalf.
Better Safe Than Sorry
The Care and Support Statutory Guidance identified that not all cases of self-neglect need to go to Section 42 enquiry – perhaps the situation is not impacting on the person’s wellbeing, does not impact on others, or is not a result of abuse or neglect.
It could be argued that someone self-neglecting is not going to share intimate details of themselves straight away. It can take time to develop trust and unless further enquiries are made (often requiring a multi-agency response to information gathering and capacity assessments) we may be leaving someone vulnerable, and making assumptions that cannot be justified later.
The purpose of a safeguarding enquiry (Section 42) is initially for the local authority to clarify matters and then decide on the course of action to:
- Prevent abuse and neglect from occurring
- Reduce the risk of abuse and neglect
- Safeguard in a way that promotes physical and mental wellbeing
- Promote choice, autonomy and control of decision making
- Consider the individual’s wishes, expectations, values and outcomes
- Consider the risk to others
- Consider any potential crime
- Consider any issues of public interest
- Provide information, support and guidance to individual and organisations
- Ensure the people can recognise abuse and neglect and then raise a concern
- Prevent abuse/neglect from reoccurring
- Fill in the gaps in knowledge
- Coordinate approaches
- Ensure that preventative measures are in place
- Coordinate multi-agency assessments and responses
These responsibilities apply to people who hoard/self-neglect and whose health and wellbeing are at risk as a result. People may not engage with professionals or be aware of the extent of their self-neglect.
For social workers and health professionals, this provides a significant challenge in developing relationships that empower the individual, or safety plans based upon what makes a person feel safe and well cared for, yet respect autonomous decision making, while juggling other duties and responsibilities.
It is important to explore with the person their history; listen to the way they talk about their life, difficulties and strategies for self-protection.
By doing this social workers can begin assessing why the person self-neglects and offer support in replacing attachment to objects with interaction and relationships with people and the community. Distress may lead people to seek comfort in having possessions; when faced with isolation they may seek proximity to things they’re attached to and when faced with chaos may seek to preserve predictability.Early relationships can have quite an effect on how a person perceives the world and may not recognise their self-neglect and may even find comfort in the situation. Deep-seated emotional issues, which have evolved as coping strategies cannot be undone in an instant.
Trauma Informed Practice should be considered.
9. Top Tips
9.1 Myth busting
| Myth | Fact |
| Self-neglect is about hoarders | Self-neglect includes lots of other factors, such as not managing personal care or medication, not paying bills or eating properly. Many people who hoard don’t self-neglect at all. |
| We (social worker, nurse, psychologist, occupational therapist, mental health team etc) can wave a magic wand. | We can help but the person needs to engage with what is offered. |
| Medication and therapy can provide a quick solution. | Improving wellbeing, quality of life or neglectful behaviour can take a long time. |
| Safeguarding will sort everything out (an easy referral can keep this person safe). | It’s a team effort. It requires a multi-agency approach to work with complex cases. |
| If a safeguarding referral is made, the social worker can enter a person’s home and remove self-neglecting people from their property. | Social workers are unable to remove someone from their property without consent or a court order or legally prescribed process. |
| People can be forced to engage in personal care tasks and have support from care agencies. Staff can ‘just do it’ for the person and fix the problem. | A person has to consent to personal care being undertaken. If someone has mental capacity they have the right to make unwise decisions. |
| f a person refuses help, such as with de-cluttering or cleaning, we can force them to accept it. | It is all about negotiation and understanding why they are saying no, and an attempt to reach a shared goal so some support can be delivered and the risk reduced. |
| Social workers can over-ride someone’s decision when they have mental capacity. | They cannot, nobody can. |
| Social workers have powers of surveillance. | They don’t. |
| Only doctors can assess mental capacity. | A range of people can assess capacity, depending on how well they know the person and what the decision is that needs to be made. |
| Self-neglecting people are lazy and it’s a ‘lifestyle choice’. | Situations can be very complex, and it may be choice in some elements of the adult situation, but not all. |
9.2 Effective engagement
| Ask the person to tell you a story about them or their past |
| Take note of objects around them, such as photographs and jewellery and engage in conversations about specific items |
| Ask them what helps when things get difficult |
| Find out information about the person’s past, and how this may trigger their behaviour in the present |
| Have an open and honest conversation and ensure their response has been acknowledged |
| Body language – don’t look shocked or uncomfortable, be open and positive, be mindful of your facial expression |
| Ask what their current concerns are |
| Ensure you display empathy |
| Consider how you would speak to the person if they were your friend |
| Look into the person’s support networks, including friends and family. Find out about any interests they have, or have had previously |
| Ask them what they would like to accomplish in the future |
| Go at the person’s own pace |
| Find out what the individual wants help with, this may not be related to their self-neglect |
| Be clear about what can happen |
| Encourage a deeper conversation, for example ‘what are the things working well in your life?’ |
| Ask them what you can work on together to achieve what they want from their life |
| Set milestones, keeping them small and timely, for example ‘what hopes do you have for the coming week?’ |
| Ensure you are in a location where the person feels comfortable to talk, which may not always be at home initially |
| Offer an understanding statement, for example ‘I understand that the problem with your neighbours is really affecting you’ |
| Write down some key points before entering the conversation |
| Identify the strengths in the person that you might highlight in your conversation and how some ideas on how they might draw on those strengths |
| Appreciate their circumstances and tell them you want to learn about them, such as asking about their strengths, abilities and preferences. |
9.3 Professional curiosity
- Offer to make a cup of tea, whilst doing so, see if there is enough food in the cupboards and fridge.
- Ask to see where they sleep; is it easy to access? Are the sleeping arrangements appropriate for that person?
- Ask if they feel safe living where they are. If they say ‘no’, explore why.
- Find out how they keep themselves warm. Discuss heating arrangements.
- Give the person time to answer the question. Allowing for silence when they are thinking.
- Never make assumptions without talking to the individual or fully exploring the case.
- Use your communication skills, review records, record accurately, check facts and feedback to the people you are working with and for.
- Focus on the need, voice and the lived experience of the person.
- Listen to people who speak on behalf of the person and who have important knowledge about them.
- Speak your observations such as ‘I’ve noticed you’ve lost weight, have you been feeling unwell’?
- Pay as much attention to how people look and behave as to what they say.
- Build the foundation with the person before asking more personal and difficult questions.
- Ask ‘How are you coping at the moment?’ ‘What helps when you are not feeling your best?’
- Explore the person’s concerns. Don’t be afraid of asking why they feel a certain way.
- Put together the information you receive and weigh up details from a range of sources and/or practitioners.
- Ask yourself ‘How confident am I that I have sufficient information to base my judgements on?’
- Question smoking habits, and consider fire risk at the same time, such as ‘Where in the property do you smoke the most?’ ‘Is it in bed or the living room?
- Speak to the person about medications. Ask if they are taking medication and how they find it. Do they have side effects, are they taking it consistently?
- Ask who visits and how long it has been since they had a visitor.
- Ask if they are in any pain, and what they are doing to manage the pain?
- Ensure the person feels listened to and valued. When ending the conversation, thank them for sharing with you.
See also Professional Curiosity chapter.
10. Further Resources
Care Act 2014 Section 42 – Enquiry by Local Authority
Care Act 2014 Section 47 – Protecting Property of Adults
Ten Top Tips when Working with Adults who Hoard (Community Care)