1. Introduction
Safeguarding concerns can be raised regarding adults within any care setting. Where safeguarding concerns are raised about an individual these should be progressed via a Section 42 Enquiry (see Stage 2: Enquiry) where they meet the criteria as set out in the Care Act, Section 18.
Provider concerns refer to issues that affect a group of people who receive care from a Local Authority commissioned care provider. The outcome of any individual Section 42 Enquiry related to such a care provider should be fed back through this Provider Concerns process. The Provider Concerns process should only be invoked where there are patterns of safeguarding concerns that indicate that the provider has not made any changes to reduce the number of incidents surrounding the same or similar situations and there is concern that the provider is unable to provide care and support in a safe environment that respects the human rights of people in receipt of that care.
2. Organisational Abuse
Organisational abuse (or organisational safeguarding) is a broad concept and is not just applicable to high profile cases, for example Winterbourne View. It is an umbrella term defined as, ‘the mistreatment or abuse or neglect of an adult at risk by a regime or individual’s within settings and services that adults at risk live in or use, that violate the person’s dignity, resulting in lack of respect for their human rights.’
Organisational abuse occurs when the routines, systems and regimes of an institution result in poor or inadequate standards of care and poor practice which affects the whole setting and denies, restricts or curtails the dignity, privacy, choice, independence or fulfilment of adults. Organisational abuse can occur in any setting providing health and social care. A number of inquiries into care in residential settings have highlighted that organisational abuse is most likely to occur when staff:
- receive little support from management;
- are inadequately trained;
- are poorly supervised and poorly supported in their work; and
- receive inadequate guidance.
3. Early Identification
Hull University (Abuse in Care Project, 2012) identified over 90 individual indicators or warning signs for concern. A summary of factors which can increase the likelihood of abuse occurring within provider settings are drawn from these indicators:
- management and leadership;
- staff skills, knowledge and practice;
- residents’ behaviours and wellbeing;
- the service resisting the involvement of external people and isolating individuals;
- the way services are planned and delivered;
- the quality of basic care and the environment.
Where there is proof or suspicion of organisational abuse by omission, for example the abuse and neglect highlighted in the Winterbourne View and the Old Deanery reports, or omission to provide care and support that puts adults at risk of or experiencing abuse or neglect, action will be channelled through this Provider Concerns process.
4. Principles
The following principles apply to the Provider Concerns process:
- the safety and wellbeing of adults using the service is paramount;
- strong partnerships that acknowledge the expertise of others;
- openness and transparency to achieve positive outcomes;
- joint accountability for risk between commissioners, safeguarding leads, providers, the police, the local authority, the ICB and other stakeholders who may be involved;
- prudent targeted use of resources;
- information is shared responsibly between all agencies, including the provider;
- cooperation between agencies;
- natural justice.
How concerns are addressed depends on level of risk and the impact on people using the service. There are no hard and fast rules, and each case should be considered on its own merit. The process can challenge capacity of one service /organisation therefore it is important that there is a shared approach, breaking down barriers between services and organisations to provide a joined up, one team approach.
5. What is a Provider Concern?
The provider concerns process can relate to both contracted providers and non-commissioned providers. We have to acknowledge the difference between individual safeguarding concerns, assessment and investigations within a provider setting to that of concerns impacting on a larger group of individuals within that setting.
Additionally we must recognise the difference between issues that would be dealt with through normal contract management processes and what should be escalated under the Provider Concern Process and could ultimately constitute organisational abuse.
6. The Provider Concerns Process
The South Tyneside Safeguarding Children and Adults Partnership sets out a range of circumstances as to when the process should apply. Provided below are some working examples:
- a number of safeguarding concerns raised for similar issues, within a few months of each other in respect of individuals who are receiving care from the same provider;
- a combined number of safeguarding concerns across a set of group homes owned by the same organisation;
- inappropriate recruitment processes or staffing levels;
- lack of, or unsuitable care plans.
In order to clarify these matters further we need to consider and establish what the working threshold level is for applying the provider concerns process. This is best achieved through the assessment of risk and is something which we will look at in more detail in the sections to follow.
6.1 Provider Concerns Threshold Level
At times it is difficult to decide whether or not a provider should go into provider concerns. Consideration should be given to the associated risk. Appendix 1, Provider Concern Process Flowchart and Appendix 2, Provider Concerns Threshold Table provide a summary and demonstrate combined threshold levels, as an indication as to how concerns should be managed.
It is important to view each situation on a case by case basis, collating inter-agency intelligence and utilising specific risk assessment processes. Risk can and should be considered at various stages of the process. The risk assessment tool can be used to compile information to help decide whether a provider should go into serious concerns or it can be use throughout the process to monitor and mitigate risk. The risk assessment will cover safeguarding considerations and compliance information; it will also include a specific risk analysis of the provider and the current situation.
It is best to collate multi-agency information and gain an agreement as to the risks involved and whether to take the matter forward through the provider concerns process. It may be beneficial to use this to evidence the level of concern prior to initial decision making. It must be acknowledged that the collection of information must not delay initial conversations.
Where concerns are growing but not yet serious and time allows the provider intelligence meeting can be used, alternatively a decision from a responsible officer is required. If at this point the responsible officer feels matters are still unclear then the case should go into provider concerns and the decision taken at the initial meeting.
7. Roles and Responsibilities
7.1 Host authority
The local authority in the area where abuse or neglect has occurred is the host authority.
The host authority is responsible for:
- liaising with the regulator if any concerns are identified about a registered provider;
- determining if any other authorities are making placements, alerting them and liaising with them over the issues in question / under investigation;
- coordinating action under safeguarding and has the overall responsibility to ensure that appropriate action is taken and monitoring the quality of the service provided;
- ensuring that advocacy arrangements are in place where needed, and care management responsibilities are clearly defined and agreed with placing authorities;
- ensuring that there is a chair and administration of meetings, and provides a clear audit trail of agreements, responsible leads for particular actions and timescales;
- taking on the lead commissioner role in relation to monitoring the quality of the service provision.
7.2 Placing authority
The local authority that has commissioned the service for an individual/s delivered by a provider where there is a provider concern.
The placing authority is responsible for:
- duty of care to people it has placed that their needs continue to be met;
- contribute to safeguarding activities as requested by the host authority, and maintain overall responsibility for the individual they have placed;
- ensure that the provider, in service specifications, has arrangements in place for safeguarding;
- the placement continues to meet the individual’s needs;
- undertaking specific mental capacity assessments, or best interest decisions for, individuals they have placed;
- reviewing the contract specification, monitoring the service provided and negotiating changes to the care plan in a robust and timely way;
- all usual care management responsibilities;
- assessments under the Deprivation of Liberty Safeguards;
- keeping the host authority informed of any changes in individual needs and/or service provision.
7.3 Care Quality Commission
The Care Quality Commission (CQC) acts independently. It is a valued partner in the process of information sharing and working to tackle areas of concern. Its expertise in working with providers and standard setting may support safeguarding processes. The CQC has the authority to take appropriate enforcement action where providers are found to be slipping, but have not yet breached the requirement. This supports the CQC’s approach to inspection and enforcement which is based less around compliance of set outcomes, and instead focuses on five key questions about care, the Fundamental Standards:
- Is it safe?
- Is it effective?
- Is it responsive?
- Is it caring?
- Is it well led?
Where there has been a recent inspection it may be helpful for providers to share pre-publicised reports, to support the principle of openness and transparency. In some instances providers may be addressing issues identified by inspections and adult safeguarding and it makes sense to address both through agreed joint processes.
7.4 Local authority
In most cases, the local authority will lead on safeguarding action in consultation with partners and in particular regulators. The principle on who is best to lead on an enquiry should always be determined by the issue, who the lead commissioner is and the knowledge and expertise required.
7.5 North East and North Cumbria Integrated Care Board
The Integrated Care Board (ICB) should be informed where there are a number of individual safeguarding concerns regarding people within a health commissioned service. The ICB will progress these concerns through the Quality Review process.
7.6 Police
As with all criminal matters the police are the leads and must be consulted about any additional proposed action.
7.7 Frontline workers
Throughout the safeguarding processes a number of tasks and actions will be identified. The table below contains suggested roles, although action should always be determined on a case by case basis and the best qualified person to assess or assure the issue assigned. A system whereby professional knowledge and skills complement each other is the most effective way to safeguard people.
| Social workers / managers
Care managers
Reviewing officers
Contract monitoring officers
Commissioners |
Review care plans and risk assessments
Analyse staff rotas
Check incident / accident reports
Review policy and procedures
Mental capacity and DoLS audits |
| Nurses
Occupational therapists
Physiotherapists
Behavioural therapists
Pharmacists |
Infection control
Review nursing and treatment plans
Manual handling assessments
Safety and use of equipment e.g. hoists
Falls policies and strategies to reduce falls
Medicine management |
| General Practitioners |
Primary health care
Raising safeguarding concerns |
| Northumbria Police Service, Community Safety Unit |
Criminal investigations
Wilful neglect
Provide expertise on investigative practice
Crime prevention visits |
| Legal services |
Advice where there are legal challenges to safeguarding or contractual matters
Advice on decommissioning decisions |
| Adults who use services |
Raising concerns and complaints
Monitoring improvements |
| Advocates
Family / friends / visitors |
Supported decision making
Consulted on best interest decisions
Raising concerns, monitoring improvements |
8. Defining Roles, Responsibilities and Process
Various numbers of professionals and agencies may be involved with individuals and their care provider, all in a position to identify potential serious concerns. We will look at the key groups of professionals involved at a local level, how they interact with the process and consider how they operate to safeguard individuals, improve the quality of service delivery provided in our Borough and identify potential serious concerns.
Practitioners from all social work teams are in a key position to monitor the care environment across all types of contracted provision, assess the quality and delivery of provider care plans, provide early notification to quality and commissioning officers in relation to compliance and quality issues or report safeguarding concerns.
Practitioners (from all teams) are responsible for ensuring that provider care plans and the actual delivery of care addresses the needs established during the assessment and are in accordance with the social care/health support plan. Re-assessments must be conducted jointly with the care provider and changes to provision must be reflected in both the revised social care support plan and the provider care plan.
Where care planning and delivery is failing practitioners should raise the issues with the care provider. Practitioners are responsible for reporting any identified safeguarding issues and engaging appropriately with the ongoing process. Where issues are related to contract compliance or quality concerns the practitioner must inform the commissioning team as appropriate and work with them accordingly.
Line managers and / or Assistant Team Managers must be informed of arising issues. In turn they make the initial decision as to whether these issues should be shared through the multi-agency monthly provider intelligence meeting, or should be progressed immediately to the Provider Concern Process.
The Let’s Talk Team (see Local Contacts) manage all safeguarding concerns and capture the information presented through the initial contact. This in turn is forwarded on to the relevant Adult Social Care Manager who is responsible for investigating concerns raised in relation to adults at risk. Within the first 24 hours, the duty manager evaluates the situation and decides whether to progress through the recognised safeguarding processes. Any safeguarding alerts that include a provider as an alleged perpetrator will be progressed via the Safeguarding Team.
The Let’s Talk Team play a crucial role in collating and interpreting information from various sources to build up a picture of what is happening across our contracted care providers. Working in conjunction with key partners they take a preventative approach, working to support and educate providers thus stopping issues escalating into what would be considered as serious provider concerns. Where the threshold for provider concerns has been reached the safeguarding team form a part of the multi-agency response.
9. Adults who use Services / Carers / Advocates
As with Section 42 enquiries it is essential that adults using the service are spoken to, and encouraged and supported to:
- tell us what outcomes they want
- raise complaints and concerns;
- questioning when care is not provided according to care plans;
- care is not delivered when expected; or
- care is not provided with dignity and respect.
Where there are patterns of complaints and concerns these may indicate poor quality service or a safeguarding concern.
10. Differentiating between Poor Care and Potential Safeguarding Issues
10.1 Poor care
Poor care, includes instances of:
- a one-off medication error (although this could have had very serious consequences);
- an incident of under-staffing, resulting in a person’s incontinence pad being unchanged all day;
- poor quality, unappetising food;
- one missed visit by a care worker from a home care agency.
10.2 Potential causes for concern
Potential causes for concern, include instances of:
- a series of medication errors;
- an increase in the number of visits to A&E, especially if the same injuries happen more than once;
- changes in the behaviour and demeanour of adults with care and support needs;
- nutritionally inadequate food;
- signs of neglect such as clothes being dirty;
- repeated missed visits by a home care agency;
- an increase in the number of complaints received about the service;
- an increase in the use of agency or bank staff;
- a pattern of missed GP or dental appointments;
- an unusually high or unusually low number of safeguarding alerts.
There should be careful analysis to understand what is intentional and unintentional harm. However, where there is unintentional harm due to lack of guidance for staff this may also constitute organisational abuse.
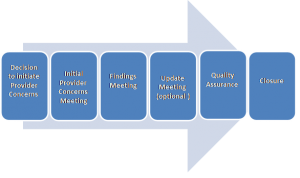
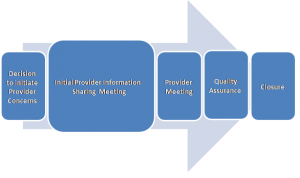
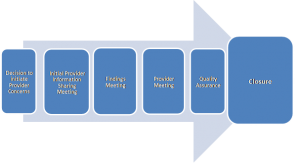
Appendix 1: Provider Concerns Process Flowchart
Click here to view Provider Concern Process Flowchart
Appendix 2: Provider Concerns Threshold Table
Click here to view Provider Concerns Process
Appendix 3: Provider Intelligence Meeting (Domiciliary Care and Care Homes)
Sharing information on quality and safeguarding, strengthening the relationship and knowledge sources from commissioning, safeguarding, CQC, ICB and front line practitioners assists in driving up standards. Formal mechanisms for sharing information between agencies are helpful to determine risk levels and the most proportionate response. The purpose of such mechanisms is to ensure both soft and hard intelligence, available agencies is brought together in an effective and cohesive manner to facilitate timely action.
South Tyneside local authority has implemented a formal intelligence meeting, with key partners from the CQC and the ICB. The ‘Provider Intelligence Meeting’ has the ability to:
- reduce the need for safeguarding under Provider Concerns procedures;
- enhance the standards of care and support by sharing early warning signs with providers;
- target resources effectively to reduce duplication;
- support prevention strategies;
- support continuous service improvements.
3.1 Liaising and reporting to the police
Information arising from these meetings should always be provided to the police where there is an indication of possible crime. It may also be prudent to have police presence at such meetings, so that they can make an early assessment. Local protocols will determine how information is shared with the police.
Thanks for your feedback!